the prostate gland is located inferior to what structure?
Achieve Mastery of Medical Concepts
Table of Contents
Development
- The prostate arises from epithelial buds that sally from the embryonic urogenital sinus.
- The buds elongate and split, becoming hollow, forming the ducts and acini.
- Interfascicular fibroblasts and the smooth musculus of the prostate arise from the urogenital sinus mesenchyme.
- The prostatic Müllerian mesenchyma farther differentiates in response to stimulation with male androgen hormones, forming the prostate.
Gross Beefcake
Structure of the prostate
- Lobular fibromuscular gland, covered in a gristly capsule, surrounding the prostatic urethra from the bladder base to the external urethral sphincter, where the membranous portion of the urethra begins
- Boilerplate dimensions: 3 cm long, iv cm wide, and 2 cm in anteroposterior (AP) depth
- Located in the lesser pelvis and lies immediately:
- Junior to the bladder
- Posterior to the pubic symphysis
- Anterior to the rectum
- Consists of both muscular and glandular tissue:
- The glandular part makes upwards approximately ⅔ of the prostate; the other ⅓ is fibromuscular.
- Glandular tissue can exist subdivided into iii singled-out zones, which produce secretions that brand up approximately twenty% of the seminal fluid.
- Main prostatic glands: brand up the peripheral ⅔ of the gland and empty into the distal urethra
- Submucosal (outer periurethral) glands: empty into the urethral sinuses
- Mucosal (inner periurethral) glands: empty directly into the urethra
- The prostate gland is divided anatomically into 5 lobes:
- An anterior lobe (isthmus):
- Located anterior to the urethra
- Fibromuscular: the muscle fibers that are a superior continuation of the external urethral sphincter to the bladder neck
- Contains picayune, if any, glandular tissue
- A posterior lobe:
- Posterior to urethra
- Junior to ejaculatory ducts
- 2 lateral lobes: located on either side of the urethra
- ane median lobe: cone-shaped portion of the gland situated betwixt the 2 ejaculatory ducts and the urethra
- An anterior lobe (isthmus):
- The prostate consists of histologically different areas; on this basis, the gland is divided into 4 zones:
- The key zone:
- Information technology forms the base of the gland.
- Encircles the ejaculatory ducts
- 25% of glandular tissue
- The peripheral zone:
- Encircles most of the fundamental zone and partially surrounds the distal office of the prostatic urethra
- Almost prostate cancers arise from the peripheral zone.
- 70% of this zone is made up of glandular tissue.
- The transition zone:
- Encircles the portion of the urethra between the urinary float and verumontanum
- 5% of glandular tissue
- The anterior fibromuscular stroma:
- This area has no glandular tissue.
- Consists of by and large muscular and fibrous tissue
- The key zone:
- The urethra enters the prostate near its anterior border and passes between its anterior and center thirds.
- The ejaculatory ducts laissez passer through its posterior region to open into the prostatic urethra.
-
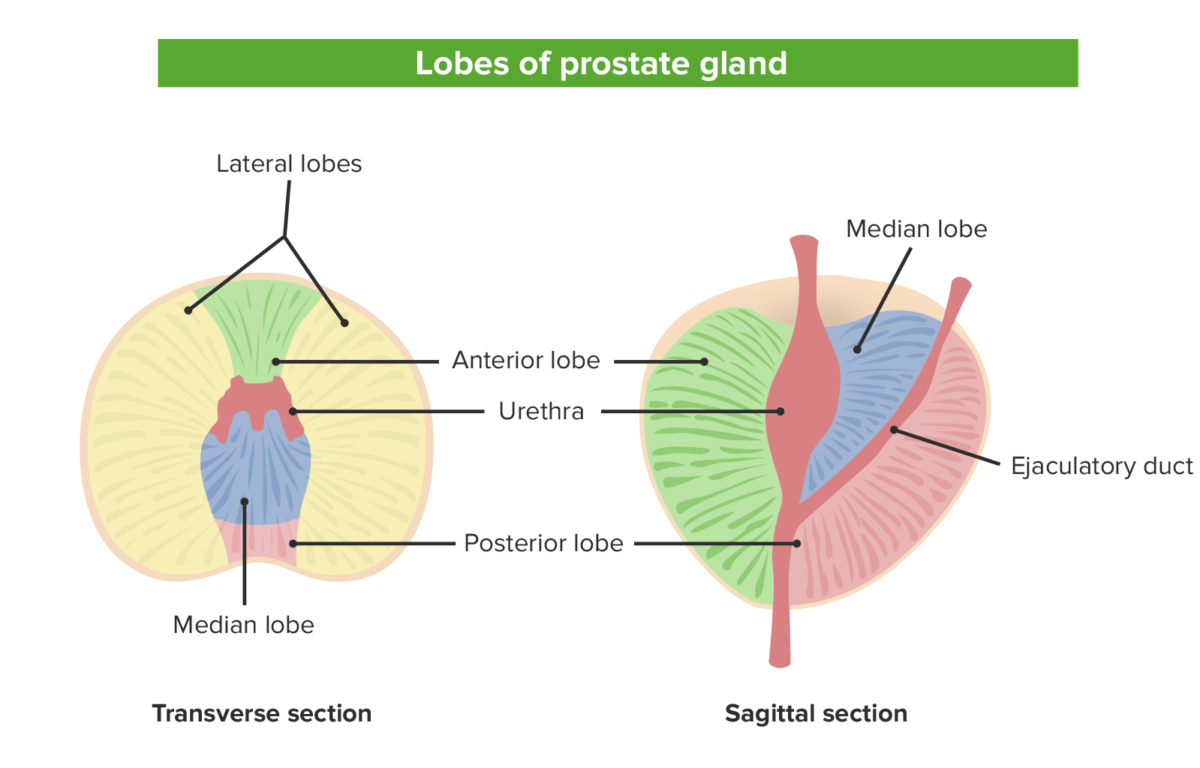
The 5 lobes of the prostate from both the sagittal view on the left and the transverse view on the correct: Note the relationship between the various lobes and the locations of the urethra and ejaculatory duct.
Image past Lecturio. -
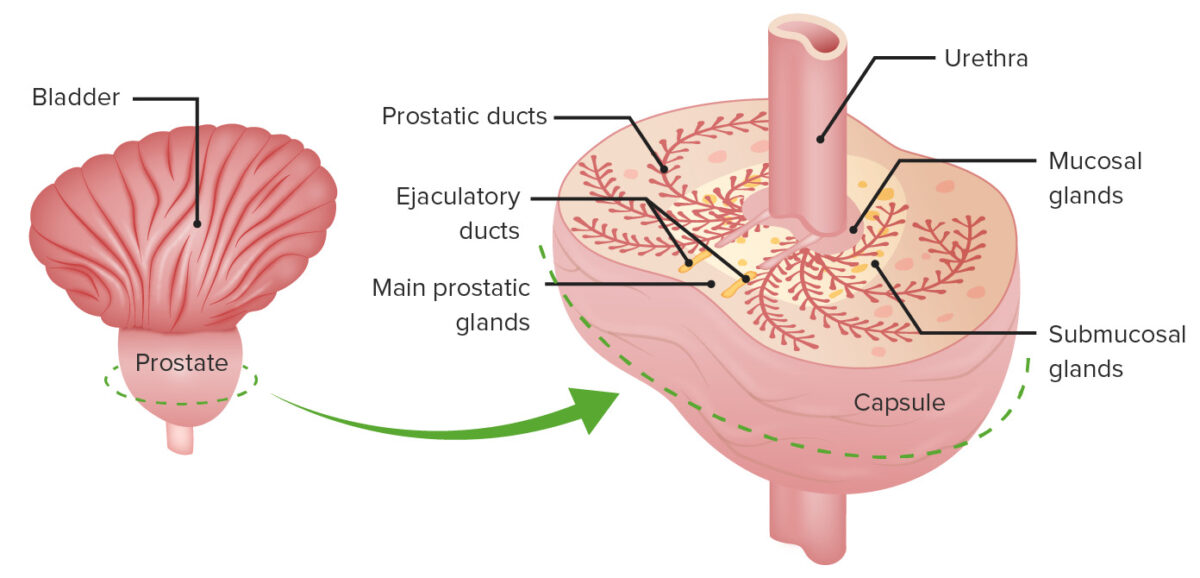
The different zones: the mucosal gland that surrounds the prostatic urethra, the key submucosal glands, and the peripheral primary prostatic glands
Prototype by Lecturio.
Accessory glandular structures
- Seminal glands (vesicles):
- Elongated construction, approximately v cm long
- Lies betwixt the fundus of the float and the rectum
- The duct of the seminal gland joins the ductus deferens to form the ejaculatory duct.
- Secrete a thick alkaline fluid with fructose (an energy source for sperm)
- Bulbourethral glands (Cowper'south glands):
- Pocket-size lobulated structures located immediately posterior and lateral to the bleary urethra and superior to the perineal membrane
- Wrinkle of muscle fibers leads to the expulsion of articulate mucus from the glands during sexual arousal.
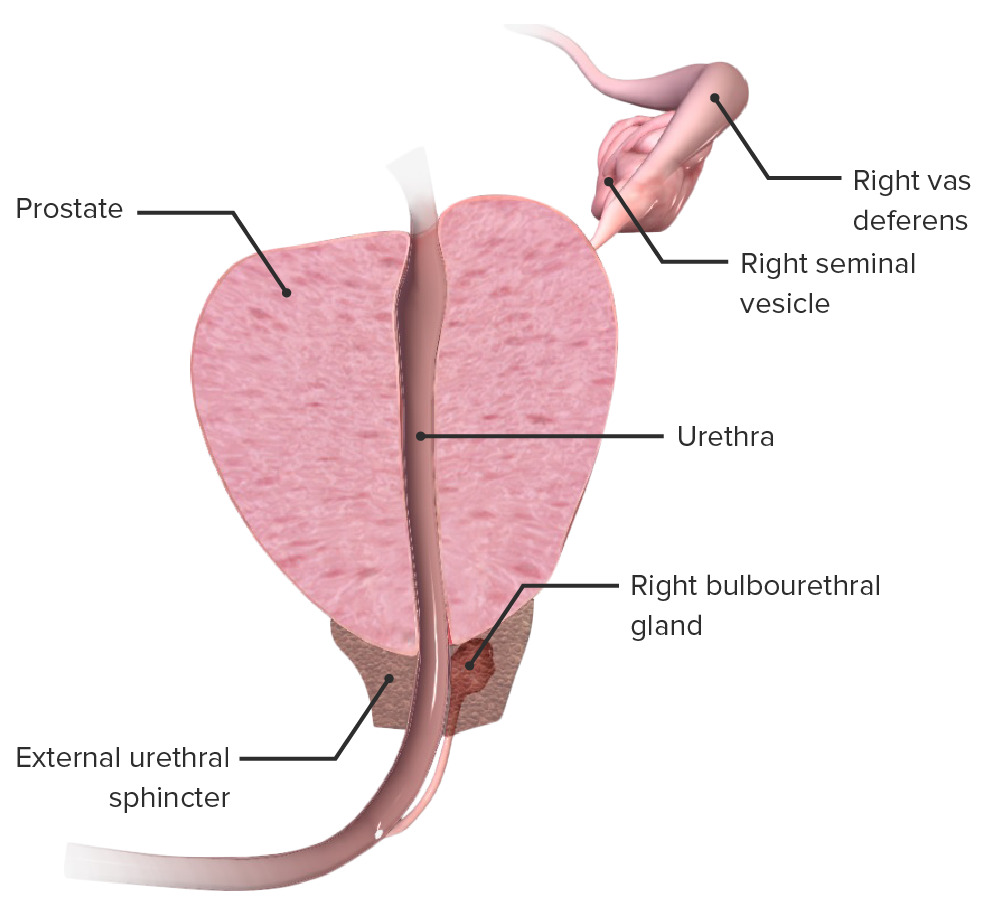
Anatomy of the prostate:
Cross-department of the prostate demonstrating its relation to the prostatic urethra, urethral sphincter, seminal vesicles, and bulbourethral gland
Neurovasculature and Lymphatics
Arterial supply
Blood vessels supplying the prostate ascend from the internal iliac avenue and enter the gland from the posterolateral region.
- The iliac avenue gives ascension to inferior vesical.
- The inferior vesical gives ascension to ii branches:
- Urethral branch
- Capsular branch
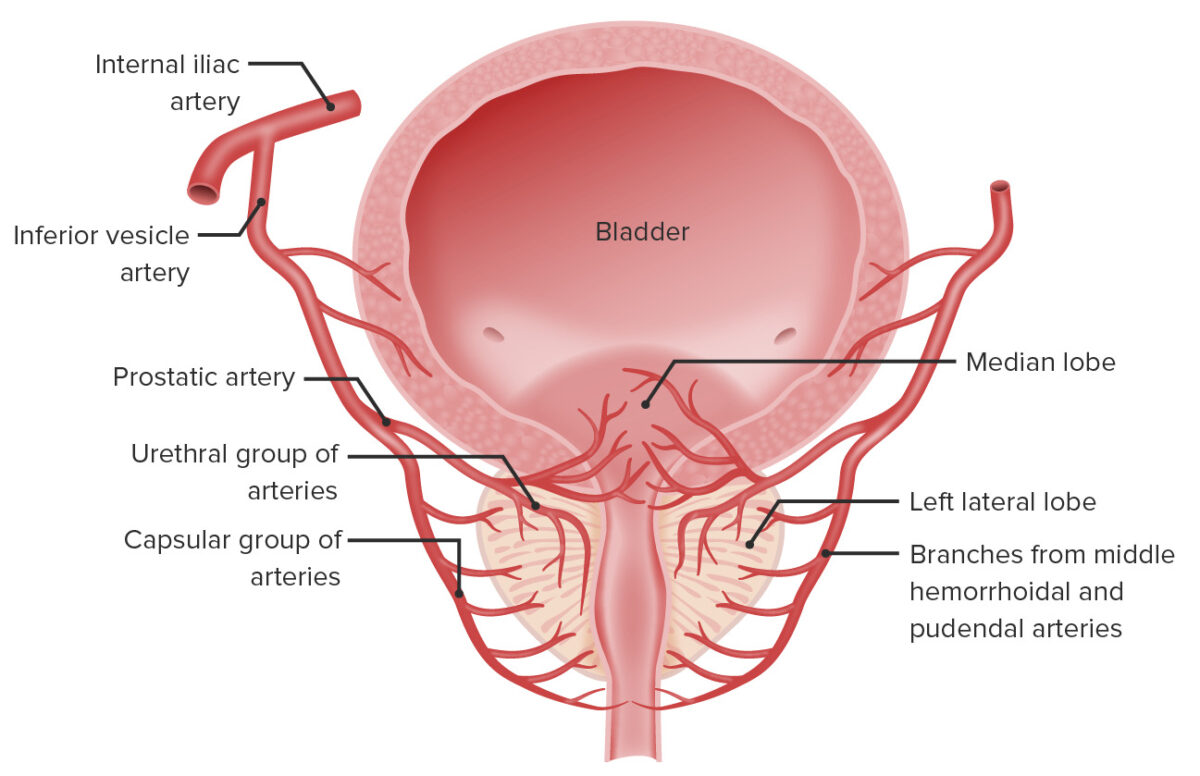
Anatomy of the vascular supply of the prostate and bladder:
The arterial blood supply of the prostate and bladder originates from the internal iliac avenue, which gives off the inferior vesicle artery. This in plow gives ascension to the prostatic artery, which branches in urethral and capsular groups which feed those portions of the prostate.
Venous drainage
- The veins surrounding the prostate join to form the prostatic venous plexus around the sides and base, which drains into the internal iliac veins.
- The prostatic venous plexus is continuous superiorly with the vesical venous plexus.
- The prostatic venous plexus communicates posteriorly with the internal vertebral venous plexus.
Lymphatic drainage
- Internal iliac lymph nodes
- Sacral lymph nodes
Innervation
- The prostate is innervated by autonomic fibers arising from the inferior hypogastric plexus:
- Sympathetic innervation from the hypogastric nerve
- Parasympathetic innervation via the pelvic splanchnic nerve
- Sensory innervation is provided by the hypogastric and pelvic plexuses.
- Urethral sphincter motor innervation is supplied by somatic pudendal nerve fibers.
Microstructure
The prostate consists of glandular tissue and fibromuscular tissue.
- Glandular epithelium is arranged in acini and ducts lined by:
- Luminal cells:
- Columnar, with pale eosinophilic cytoplasm and circular nuclei
- Secrete into the lumen, contributing to seminal fluid product
- Strongly positive for PSA immunohistochemistry
- Basal cells:
- Basement membrane adjacent
- Ovoid nuclei and inconspicuous cytoplasm
- The number of basal cells varies between glands in an individual prostate.
- Neuroendocrine cells: positive for neuroendocrine markers such as chromogranin and synaptophysin
- Luminal cells:
- Prostate secretions (along with seminal vesicular secretions) form the majority of the seminal fluid. Acidic secretions are composed of:
- Proteolytic enzymes
- Acid phosphatase
- PSA
- Fibrinolysin
- Zn
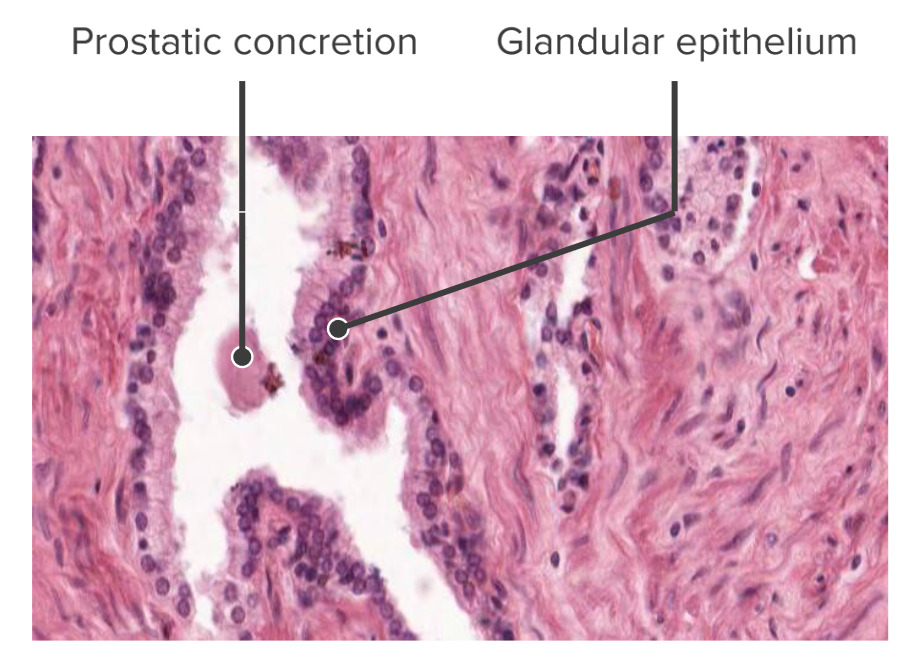
The glandular columnar epithelium of the prostate gland (histological):
Note, on this slide, the prostatic concretion; these concretions can accept a clinical application if they build upwards and impinge on the urethra → difficulty urinating
Clinical Relevance
- Beneficial prostatic hyperplasia (BPH): a common condition in older men (> fifty) characterized by a firm enlargement of the lateral and eye lobes. The growth is not premalignant and presents low levels of clinical risk. The near important symptoms include increased frequency of urination and slowness or dribbling of the urinary stream. Benign prostatic hyperplasia is detected via both blood PSA test and digital rectal exam (DRE). Various handling options are available, including surgical and supportive.
- Prostate cancer: among the about mutual cancers in men worldwide. Prostate cancer may cause no signs or symptoms in its early stages. Exceptionally, the cancer may present with nonspecific urinary symptoms, hematuria, or hematospermia. Diagnosis is based on PSA testing and DRE. A variety of handling options are available, including surgery, chemotherapy, and radiation. The overall v-year survival rate is over 98%.
- Prostatitis: a term that indicates inflammation of the prostate, which can be due to infectious or noninfectious causes. Bacterial prostatitis is easier to identify clinically and its management is amend established. The main diagnostic tools for prostatitis are clinical history and physical test. Prostate massage past DRE is just recommended in patients with chronic prostatitis and non for astute bacterial prostatitis.
References
- Drake, RL, et al. (2020). Affiliate v: Pelvis and perineum. In Gray'south Anatomy for Students, quaternary Edition. Pages 467–468. Churchill Livingstone/Elsevier.
- Moore, KL, Dalley, AF, & Agur, AMR. (2014). Chapter 3: Pelvis and perineum, pelvic viscera. In Clinically Oriented Beefcake (7th Ed.). Pages 377–382. Lippincott Williams & Wilkins, a Wolters Kluwer business.
- Ittmann Thousand. (2018). Beefcake and histology of the man and murine prostate. Cold Bound Harbor Perspectives in Medicine. Retrieved Sep ix, 2021, from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5932577/
- Singh, O. (2021). Anatomy, belly and pelvis, prostate. Statpearls. Retrieved Sep ix, 2021, from https://www.statpearls.com/ArticleLibrary/viewarticle/27831
jonesmarobluns1980.blogspot.com
Source: https://www.lecturio.com/concepts/prostate-and-other-male-reproductive-glands/
0 Response to "the prostate gland is located inferior to what structure?"
Post a Comment